On this page
- Report Highlights
- Oregon Initiated Contact Tracing Early in the Pandemic
- Contact tracing teams did not keep up with the high number of cases
- Wraparound services that support isolation and quarantine can be difficult to access
- County's experience with contact tracing can provide lessons for future emergencies
- Recommendations
- Objectives, Scope, & Methodology
- Audit Staff
- Related documents
Report Highlights
What We Found
The county's COVID-19 contact tracing program did not contact all people who were infected with COVID-19 and their close contacts, especially when case numbers were high. Contact tracing is less effective when a disease is widespread. Due to high case numbers and shifting state and federal guidance, Multnomah County Public Health stopped monitoring contacts, gathering information about contacts, and conducting individual case investigation at various points in the pandemic. Currently, outbreak investigation and support services for isolation and quarantine are the only functions remaining in the program.
Support services providers were also affected by high cases numbers. Providers were able to deliver essential services, like grocery and utility assistance, though there may have been delays during surges. Additionally, a complicated system, reliance on phone calls, and lack of advertising likely affected access to these services.
The experience of this program can be instructive for future emergencies. The county could be better prepared to quickly onboard a rapidly growing team. The county can also build on its experiences to continue to build capacity for community partnership work.
Why We Did This Audit
This audit is part of a series of pandemic response audits and was on our 2021 audit schedule. Contact tracing was an important part of the county's direct public response to COVID-19.
What We Recommend
We recommend that Health Department leadership, in partnership with the Department of County Human Services leadership, should:
- Provide better oversight and support to community-based organizations by assessing data collection and information sharing, providing more frequent education and technical support, and monitoring monthly reporting requirements.
- Create a mechanism for county staff who work with community partners to network, collaborate, and develop professionally.
We also recommend that the Chief Operating Officer work with department leadership, Human Resources, Risk Management, and Emergency Management to identify barriers and establish processes for redeploying county experts to programs in need during emergencies. They should also evaluate and adjust general county training to ensure it is readily available and addresses working during an emergency.
Oregon Initiated Contact Tracing Early in the Pandemic
The World Health Organization received information about a new viral disease in Wuhan, China in December 2019. The novel coronavirus became known as “coronavirus disease 2019,” or “COVID-19.” On January 21, 2020, the first case of COVID-19 was reported in the United States. Multnomah County activated the Emergency Operations Center a week later to coordinate a response. By the end of February 2020, the Oregon Health Authority confirmed Oregon’s first presumptive case.
On March 8, 2020, Governor Kate Brown declared a state of emergency. The “Stay Home, Save Lives” order directed people to stay at home, closed non-essential businesses, and required physical distancing measures. Shortly thereafter, the World Health Organization declared that COVID-19 was a global pandemic.
Governor Kate Brown released reopening guidelines for the state on May 7, 2020. Counties had to fulfill a variety of prerequisites before applying to reopen, including having isolation facilities, a contact tracing system, and a declining prevalence of COVID-19. The contact tracing system was required to have 15 tracers per 100,000 people, cultural and linguistic competence on the team, and the ability to trace 95% of contacts within 24 hours. In Multnomah County, this equated to 122 contact tracers.
Contact tracing includes multiple functions and purposes
Early on in the pandemic, public health agencies used the term “contact tracing” to refer to the processes of case investigation, contact tracing, outbreak investigation, and support services for isolation and quarantine. This audit covers those four distinct yet interrelated activities. These activities are defined in the box below.
From May 2020 through January 2022, the Multnomah County Health Department’s Public Health Division (Public Health) performed contact tracing and case investigation. County Public Health continued outbreak investigation after January 2022. The Department of County Human Services and community-based organizations provided wraparound services, through agreements with Public Health. Those services also continued after January 2022.
The program’s overall goals with contact tracing and case investigation were to:
- identify people who tested positive for COVID-19
- prevent transmission to others through identifying, notifying, and monitoring contacts
- improve health outcomes by providing education and resources
- collect data to better understand the disease
Four components of contact tracing:
Case investigation is the identification, investigation, and support of people who have confirmed or probable diagnoses for an infectious disease.
Contact tracing is the process of identifying, monitoring, and supporting close contacts of people who have confirmed or probable diagnoses for an infectious disease.
Outbreak investigation is the process of identifying workplaces, congregate settings, and other facilities that typically have two or more confirmed cases, identifying and correcting conditions that may have led to outbreaks, and advising facility management on control measures to decrease or stop transmission.
Wraparound services are social supports that assist people, particularly those in vulnerable populations, to safely self-isolate or self-quarantine. The support service system typically includes care coordinators, including those from community-based organizations with strong ties to groups with culturally and linguistically specific needs. At Multnomah County, support services include up to one month of grocery, utility, and rent/mortgage assistance, immediate food assistance, and isolation/quarantine accommodations.
COVID-19 has been a fast moving crisis requiring many adjustments
When the pandemic started, COVID-19 was a new disease and the health community still did not know much about it. As researchers learned new information, public health departments at all levels of government adjusted their practices and guidance. Multnomah County Public Health has some autonomy for decision-making as the local public health authority. However, the county follows state and federal guidance, which has changed frequently. Public Health has had to change procedures regularly to keep up with changing guidance.
Additionally, the potential impacts of the disease on the community have changed throughout the past two years. The county has experienced multiple "surges," or quick increases of cases in the community. New variants have changed the nature of the disease by reducing the time it takes to infect someone else. Increases in vaccination rates have reduced risks of severe disease outcomes for those vaccinated. In addition, the disease has hit some communities harder at times than others. Public Health had to adapt to changing circumstances continuously throughout the pandemic to address racial health disparities, comply with state expectations, and respond effectively.
Contact tracing is a proven public health strategy, but is it the best strategy for COVID-19?
Contact tracing is a proven public health strategy for controlling disease transmission. However, contact tracing may be less effective during the COVID-19 pandemic than other health events.
Public health departments in the United States have struggled with contact tracing throughout the pandemic. By the fall of 2020, many contact tracing teams had a hard time keeping up. With the high level of cases during the Omicron surge, many jurisdictions stopped universal case investigation and contact tracing altogether.
In January 2022, various local government and state health associations released a statement in favor of refocusing resources away from case investigation and contact tracing. And in February 2022, the CDC also stopped recommending universal case investigation and contact tracing in favor of targeted case investigation. This was in line with what was already happening at state and local levels, including Multnomah County.
So what makes the COVID-19 pandemic different from other diseases?
In a joint statement, five health associations list the following reasons for why contact tracing became less useful and feasible since the Omicron surge:
- The large number of asymptomatic and less severe cases
- Infections going unidentified by public health (through no testing or at-home testing)
- High risk of transmission before or during the first few days of symptoms
- Shorter incubation period of Omicron
To be effective, contact tracing must be done quickly. Because of the nature of the disease and the high number of cases, very few cases and contacts were traced quickly enough to disrupt transmission. While this is especially true since Omicron, we heard concerns about the effectiveness of contact tracing for COVID-19 before the Omicron surge. In all surges, delays in testing and receiving test results further slowed the process and made contact tracing less effective. Additionally, traditional contact tracing is labor intensive and expensive.
Other countries have had success with contact tracing for COVID-19, especially early in the pandemic. They have also had different situations than the U.S., with different public expectations of privacy and trust in government. Some other countries also coupled contact tracing with aggressive strategies to control community transmission. Despite challenges, many U.S. experts say that contact tracing was beneficial, especially early in the pandemic.
Contact tracing teams did not keep up with the high number of cases
Like many other jurisdictions in the United States, Multnomah County did not keep up with universal case investigation and contact tracing when case numbers were high. Case investigation and contact tracing are less effective at containing diseases when they are spreading quickly and widely. Continued high case numbers led to changes in prioritization and discontinuing some activities. The team faced additional challenges, including a mandate to use a state data system that could not handle the high volume. Public Health pivoted to respond to challenges. Ultimately, with changing circumstances, Public Health stopped universal case investigation and contact tracing. Public Health has continued outbreak investigation of high-risk settings.
Public Health discontinued case investigation and contact tracing at various times
The core functions of case investigation and contact tracing include interviewing people with positive cases, notifying people identified as close contacts, and monitoring close contacts. Case investigators and contact tracers also collect data to help understand the disease, as well as provide education and support to people with positive cases and the people they were in close contact with.
Due to large increases in cases during surges and shifting state guidance, Public Health discontinued core functions of case investigation and contact tracing at various points in the pandemic. This is not unique to Multnomah County; other public health departments in the country also discontinued elements of contact tracing at various points in the pandemic.
Public Health discontinued key steps in contact tracing during various surges
Notifying and monitoring contacts were first paused in fall 2020; case investigation ended Jan 2022
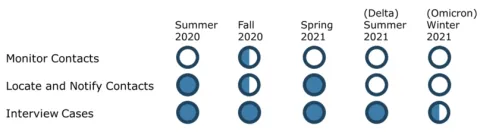
Source: Auditor assessment of county program policy changes during various surges of the pandemic. This only applies to universal individual-level case investigation and contact tracing, not outbreak investigation. Half circles represent activities that Public Health paused or discontinued part way through the surge.
Public Health stopped monitoring contacts early and never resumed
The county actively monitored contacts for only a few months during 2020. Active monitoring involves checking in with a contact via phone, text, or another method to inquire about symptoms, answer any questions, and encourage continued quarantine.
The COVID Call Center in the Department of County Human Services took on active monitoring through an agreement with Public Health for three months from September 2020 until cases surged in late November 2020. Surge protocol guidance from the State of Oregon directed public health teams to end active monitoring at that time. However, when the county was no longer operating under surge protocol, Public Health decided not to resume active monitoring.
Initially, Public Health also contracted with some community-based organizations to help with active monitoring. However, those partnerships never got going before this function ended. Public Health management reports that they decided it would be better to have the community-based organizations focus on providing support services for isolation and quarantine.
Universal contact tracing was paused in fall 2020 and ended in summer 2021
During the first large surge that started in fall 2020, County Public Health did not contact all reported cases or contacts. This was common of other jurisdictions at the time. Contact tracing is less effective at containing disease when transmission is quick and widespread. In addition, contact tracing and case investigation are resource-intensive and can be intrusive to people. The State of Oregon changed its guidance and introduced surge protocols in November 2020. In response to surges and the change in state guidance, Public Health paused universal contact tracing during fall 2020. It resumed contact tracing briefly in spring 2021, when case numbers decreased. Public Health stopped contact tracing permanently when the Delta surge hit in summer 2021 and surge protocol resumed.
After surge protocol was introduced, Public Health only went back to regular protocol for about four months in spring 2021
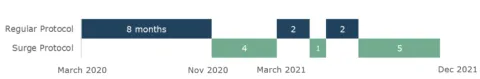
Source: Auditor assessment of documentation.
The surge protocol directed public health teams to shorten the case investigation interview and ask about fewer contacts. It directed teams to only ask about close contact with household members or people at high-risk, like people who work in care facilities or have health risks themselves. Surge protocol also directed teams to prioritize contact tracing on those high-risk contacts.
When Public Health was not doing universal contact tracing, case investigators directed people with positive cases to notify their own contacts. If anyone said they were uncomfortable notifying their own contacts, case investigators would offer to have Public Health staff notify contacts on the person's behalf. This practice did not consider whether contacts were high-risk.
Unfortunately, we were unable to access data on contact tracing. The State of Oregon mandated all counties to use the state databases Opera for case investigation and ARIAS for contact tracing. The State only shares data from Opera back with the county, not ARIAS. Therefore, we only had access to data gathered from case investigation interviews of people with positive cases. We did not have access to data gathered from contact tracers notifying people of a close contact exposure. Without that data, we do not know how many people Public Health did or did not notify about an exposure. However, since the county stopped most contact tracing during large surges, it is safe to assume most people with a close contact exposure did not receive a call from a contact tracer.
Public Health did not interview all cases during surges and stopped case investigation in early 2022
The number of COVID-19 cases reported to the county has frequently exceeded the team's capacity for universal case investigation, especially during large surges. Universal case investigation means calling and interviewing all people with positive cases to gather information and provide support and education. The nature of the disease and overall situation changed significantly between 2020 and 2022. By early 2022, state and federal authorities stopped recommending universal case investigation.
When case investigation was occurring, state guidelines stated that case investigators should call all people with positive cases. Not all people will answer their phones or be willing to participate in interviews. As the graph below illustrates, surges greatly affected the proportion of people that Public Health interviewed. According to data provided by Public Health, during the fall 2020 surge, case investigators interviewed half of people with reported cases. During the Delta surge in summer 2021, case investigators interviewed 28% of people with reported cases.
The Omicron surge started in December 2021 and led to a dramatic increase in cases that was far higher than previous surges. During the first three weeks of the Omicron surge, Public Health only interviewed 10% of cases. At this time, national public health associations recommended stopping universal case investigation due to the changing nature of the disease.
On January 6, 2022, Public Health announced that the program would stop universal case investigation and focus on investigating high-risk outbreak settings instead. Neighboring Washington and Clackamas Counties also announced that they were stopping case investigation. The State of Oregon announced an official change in state guidance to stop requiring universal case investigation on January 12, 2022. The CDC also recommended stopping universal case investigation shortly afterwards.
Public Health did not interview all positive cases reported to the county
Number of people not interviewed exceeded the number interviewed during surges
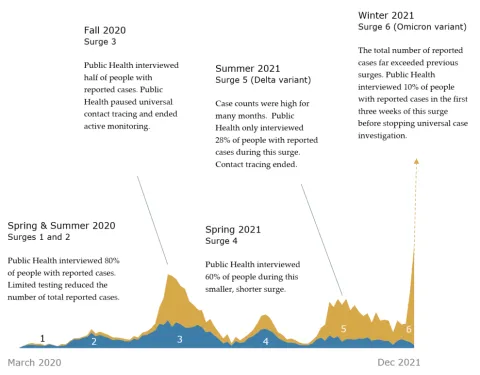
Source: Data provided by Public Health, from Opera system. Data only goes through December 2021, since case investigations ended in early January 2022. Data only includes cases that were reported to Public Health.
Outbreak sites are prioritized based on risk, with lower risk sites not always investigated
The outbreak investigation team also operated under surge protocols during periods of high case numbers. Similar to individual case investigations, the outbreak team did not investigate all reported outbreak sites. The outbreak team prioritized investigating at long-term care facilities and congregate settings. Congregate settings are places where groups of people live in shared spaces, like care homes or homeless shelters. We also heard that at times, investigators were calling outbreak sites well after the outbreak had occurred. Similar to contact tracing, we could not access outbreak data to do a full assessment. Outbreak data is stored in a subset of the state database Opera called DUDE. The state does not share data from DUDE back with the county.
Public Health quickly scaled up the team, but staffing fell short of the state's goal
Public Health quickly scaled up the contact tracing and case investigation team in summer 2020. This was a challenging task, especially in the middle of a crisis. Public Health drew on internal county staff and hired externally as well. However, the size of the team never reached the level that the state initially required for the county to reopen.
The team's size never reached the state's benchmark
Estimated number of contact tracers and case investigators by month
Source: Auditor analysis of Workday, the county's enterprise system, and organizational charts. Does not include support staff. Numbers are estimates due to limitations with Workday data. Some county staff split their time between their usual job and the contact tracing team, and their employee record did not always reflect this.
In June 2020, the state told counties that they needed to have 15 contact tracers per 100,000 people in order to reopen businesses. In Multnomah County that equated to 122 contact tracers. Multnomah County wrote in its reopening plan that it had 63 trained contact tracers in the beginning of June, with a plan to reach 122 by the end of June. The County also planned for 33 case investigation/contact tracing positions with bilingual skills.
As the graph above shows, the team size peaked in the fall 2020, below the state's benchmark. Public Health was successful at hiring a diverse workforce. At high points, the team included at least 40 staff with culturally-specific or linguistically-specific skills, some of whom were bilingual.
We heard in interviews that predicting what budget and staffing would be needed for the pandemic was challenging. While demand for case investigation usually exceeded capacity, there were slow points as well. For instance, case investigators reported having downtime in spring 2021, when cases went down after vaccinations were introduced. It was also hard to predict how vaccination would affect the need for contact tracers.
During the first fiscal year of the pandemic, FY2021, Public Health spent less on contact tracing than the county had budgeted. There were times when different response areas that share funding sources, such as testing, vaccination, and contact tracing, had greater or lesser importance. At least some of the funds went toward community testing instead. Contact tracing and case investigation are resource-intensive, and Public Health management said they had to allocate resources to where they felt they were most needed during an uncertain time. Public Health management reported that they did not prioritize contact tracing because COVID-19 was so widespread and this method had little preventative value, given their previous experiences with other communicable diseases.
For the next fiscal year, FY2022, Public Health leaders requested a smaller budget because they anticipated a reduced need for contact tracing and case investigation due to vaccines. Therefore, when the Delta and Omicron surges occurred, the county had not allocated funding that would have allowed for a larger team.
Public Health faced additional challenges and took steps to adapt
In addition to the large number of cases, Public Health faced additional challenges that limited the team's ability to perform its work. Case investigators told us that the state data system, Opera, frequently froze and crashed. This sometimes made it impossible to do their jobs. A key part of a case investigator's job is to enter the data they gather from people with positive cases into Opera. This data allows Public Health to better understand the disease. It also allows information about contacts to be sent to contact tracers. When the system crashed, case investigators could not enter this data. Some case investigators worked in the evenings when the system was less overloaded and less likely to crash.
Additionally, not everyone who tests positive for COVID-19 wants to answer a phone call from Public Health staff. Early in the pandemic, the county shared messages via social media, the county website, and local media outlets publicly encouraging people to answer case investigation and contact tracing phone calls. As time went on, people became less likely to talk to case investigators or provide contacts. Some of this could probably be attributed to pandemic fatigue. In addition, as people became more aware of guidance and information, they may have relied less on case investigators for education.
Public Health hired a diverse staff with language and cultural knowledge, skills, and abilities. This is important for creating a response that is able to connect effectively with people from the most affected communities. However, we heard that there were challenges with connecting workers with people from the communities that matched their language and cultural skills. Test results reported to Public Health did not always include data on race, ethnicity, or primary language. County employees told us that changes in state law should make race, ethnicity, and language data more available in the future.
Public Health took steps to adapt to capacity and other challenges
Public Health made program changes in response to challenges. For example, Public Health automated initial communications with cases. Some people we spoke with felt that some of these changes could have happened sooner in the process. Delays are understandable considering that Public Health was making changes while in the middle of a crisis. Additionally, Public Health management reported that they did not initially pursue some changes because of the unpredictability of the pandemic. They did not want to spend months to set up a new system that may not have been needed by the time it was ready.
However, quicker changes could have improved service delivery. For example, Public Health did not send out automated text messages until the Delta surge. If the change had happened sooner, more people would have had quicker access to time sensitive information through text messages.

Public Health implemented a new phone system in January 2021. This phone system allowed case investigators and contact tracers to call from their computers rather than a cell phone. This allowed the team to do a "warm hand off" to the COVID Call Center for wraparound services. A warm hand off is transferring a call and staying on the line long enough to know that the transfer was successful. However, even after this change, the team did not always use the new phone system because some staff preferred using cell phones. Warm hand offs are important because otherwise the call center staff have to call people back and may not reach them.

Public Health's epidemiologists also created a randomization list in response to high case numbers in August 2021, during the Delta surge. When cases were high, case investigators could not call all cases. Public Health assigned case investigators to call a random sample of the most recent cases. Focusing on recent cases is important for interrupting disease transmission. This system improved the chance that case investigators would talk to a more representative sample of people, which could improve data quality. Additionally, under this system, any one person had an equal chance of receiving education and being offered support services since they were randomly selected. However, there are limitations in how truly representative this sample could be, considering that many people are never tested or take at-home tests that are not reported to Public Health.

Public Health also adapted to data system challenges. By November 2020, the team was encountering problems with the system, Opera, freezing and crashing. At that time, management shared a hard copy of the questions that team members could use if the system was not working. In August 2021, during the Delta surge, the team switched to a fillable pdf for case investigators to fill out, rather than enter the data directly in the system. Management also hired data entry staff to input the data during evening hours when the system was more stable. We heard that by Multnomah County making this change, the system was more stable for other counties in the state. Public Health implemented this workaround months after the difficulties began.

Public Health provided a lot of public information on the county website, through social media, and community outreach. This created different avenues for the public to receive information and education about the pandemic and county services. Public Health translated or hired contractors to translate many materials into multiple languages. Public Health strived to translate core materials into five key languages. Notably, Public Health had some materials translated into 22 languages. This is far more than other counties in the metro area and on par with King County, Washington.
While Public Health's decision to translate materials into a wide variety of language is commendable, we also noticed inconsistencies in which materials were translated. Public Health typically has materials translated into the five most commonly spoken languages in the county, and languages beyond that are driven by request. This put the onus on the community to proactively ask for translations. We also heard that translations sometimes took a long time and it was hard to keep up with translations when materials change frequently.

Public Health also started sending out automated text messages and letters. This was another strategy to share information with cases about guidance for isolation, notifying contacts, and the availability of wraparound support services. This is especially important when case investigators do not call most people with positive cases . Letters were also available for people identified as close contacts. Text messages went out in English and Spanish and letters were available in multiple languages, if case investigators knew someone's primary language. Public Health also produced a guidebook with detailed information about what to do after testing. Texts and letters included links to the guide, in addition to basic information and instructions on where to call for resources.
Public Health started sending text messages in September 2021, during the Delta surge. Letters were started earlier, but Public Health initially had a hard time keeping up with mailings during surges. Starting in January 2021, the program purchased mailing services from a third party and ordered letters about twice a week. In January 2022, Public Health increased the frequency to ordering and mailing letters on most weekdays. There could have been small delays for people with positive cases to receive letters depending on when Public Health received positive test results, when Public Health placed the order, and postal delivery. This is important because information about isolation, notifying contacts, and support services is time sensitive. Public Health did not track when letters were mailed compared to test date.
The State of Oregon also implemented some tools for automation that were open to Multnomah County residents. The state rolled out a survey that people who test positive can fill out. It gathers similar information to what a case investigator would gather. The state also has a hotline to call for health information and for reporting at-home test results. These are both attempts to fill gaps in gathering information about the disease. It is not clear how often these tools are used.
Not keeping up with case investigation affects access to services
In addition to contact tracing and data collection, case investigators and contact tracers should refer people to wraparound support services to help with isolation and quarantine, as discussed in the next section. When case investigators and contact tracers do not reach cases and contacts, they may not learn about the availability of these services.
From the start of the pandemic through the end of universal case investigation in the first week of January 2022, health systems reported almost 70,000 positive test results to the county. According to Opera data provided by county epidemiologists, the case investigation team interviewed a large number of people with positive cases, around 30,000. However, for the reasons described above, that effort was not enough to keep up with the high volume.
That left almost 40,000 people with reported positive cases from March 2020 through December 2021 who did not speak with a case investigator. A case investigator did not provide them with information about how to isolate and what support services were available, or answer their questions. Since case investigation ended, tens of thousands more cases have been reported to Public Health. This is also a large undercount, since many people with COVID-19 do not get tested at all or use at-home tests and do not report those to Public Health.
For much of the pandemic people with positive reported cases received text messages and letters from Public Health with information about support services. These texts and letters will continue moving forward. People may also learn about available services through the county's website, 211, or word of mouth.
While case investigation was active, Public Health interviewed about 30,000 people and did not interview about 40,000 people
Each dark square represents about 100 people that Public Health interviewed. Each light square represents about 100 people with a reported case that Public Health did not interview.
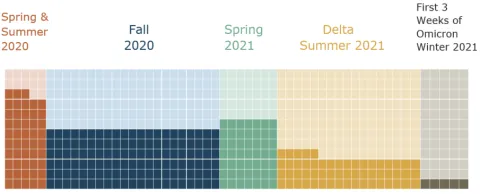
Source: Data provided by Public Health from the Opera system. Each square represents about 100 people, each with a confirmed positive test reported to Public Health. Data for the Omicron surge only goes through the end of 2021, when case investigation ended. Tens of thousands of additional cases have been reported in 2022 and are not reflected above.
Wraparound services that support isolation and quarantine can be difficult to access
County relied on new and existing partnerships
The wraparound support service system at Multnomah County evolved rapidly and in an emergency. Support services for isolation and quarantine are an essential measure to reduce or stop the transmission of COVID-19. At the beginning of the COVID-19 pandemic, the county connected with community-based organizations and community health workers in order to ensure that information, education, and services were reaching people, particularly those from vulnerable and historically marginalized communities.
Public Health had existing relationships with 17 community-based organizations that had held county contracts for community health workers to provide direct services in the past. Over the course of the pandemic, Public Health went from working with these 17 organizations to working with over 50. The Oregon Health Authority awarded state contracts to many organizations to assist with contact tracing, active monitoring, and wraparound service provision. While the number of county-awarded contracts only went from 17 to 18 in fiscal year 2022, Multnomah County awarded memoranda of understanding (MOUs) to several community-based organizations with state contracts and has involved them in wraparound service coordination and provision.
Contracts for wraparound services did not change much from FY21 to FY22
The County awarded one additional community-based organization a $100,000 contract in FY22. The other organizations were contracted for the same amount in FY22 as they were in FY21.
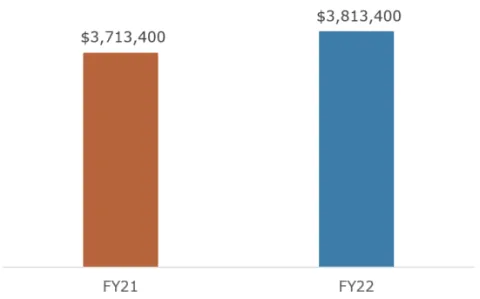
Source: Financial Data from Public Health.
Community health workers and the community-based organizations at which they work are supported by a small team within Multnomah County Public Health. This team is called Community Partnerships and Capacity Building. Community Partnerships and Capacity Building has worked with community health workers for over 10 years, and mobilized to provide trainings to current and new community health workers and partners throughout the pandemic. They manage the contracts and MOUs with community-based organizations involved in wraparound service provision.
Community-based organizations provide culturally & linguistically specific services to communities disproportionately impacted by COVID-19
Number of organizations that serve each community; some work with multiple communities.
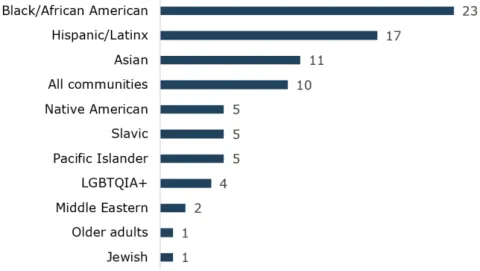
Source: Auditor analysis of data provided by COVID Call Center. This chart is a count of organizations based on the communities they indicated they serve. Many organizations work with multiple communities, so those organizations are represented in several categories.
Services evolved rapidly and the county housed them across several programs
At the beginning of the pandemic, Public Health coordinated referrals to community-based organizations. However, Public Health had limited capacity to coordinate support services for isolation and quarantine. Public Health's capacity challenges led to a large backlog of referrals to community-based organizations. Community-based organizations also reported capacity challenges such as limited resources and too many referrals. The backlog of referrals impacted the timeliness of service delivery and overall efficacy of isolation and quarantine support.
The Health Department and the Department of County Human Services entered into an interdepartmental agreement to coordinate wraparound support services. By the winter of 2020, Bienestar de la Familia (Bienestar) was providing support services and the COVID Call Center was providing immediate food assistance in addition to managing referrals to Bienestar, county health clinics, and community-based organizations.
Care coordination involves a variety of staff and external partners
Community health workers, COVID Call Center staff, and Bienestar case managers help connect community members to wraparound services.
Community health workers (CHWs) work with culturally and linguistically-specific communities, and their role includes coordinating care for people who need help safely quarantining or isolating as well as promoting individual and community health. Many CHWs who are part of the wraparound service system work at community-based organizations that have county or state contracts. CHWs have certifications and training that covers public health, interviewing, and communications. In many cases, they share culture, language, ethnicity, and life experiences with the communities they work with. In addition to connecting people to grocery, utility, and rent/mortgage assistance under the wraparound service program, CHWs provide emotional support, culturally sensitive and linguistically appropriate public health information and education, and assistance navigating other and longer-term social supports.
COVID Call Center staff are among the first points of contact with Multnomah County by people who are seeking assistance to safely isolate or quarantine. People are routed to the Call Center in many ways, such as by 211, contact tracers and case investigators, and other county phone lines. COVID Call Center staff facilitate and coordinate many aspects of the wraparound services program. They direct people to Bienestar and community-based organizations based on organizational capacity and clients' respective needs. If an individual or household needs immediate food assistance, Call Center staff place a same or next-day grocery delivery order to help people while they wait to receive additional services from Bienestar or community-based organizations. Call Center staff also provide up-to-date public health information, assistance with testing and vaccine-related information, and monitor the capacity of Bienestar de la Familia and over 50 community-based organizations to receive referrals.
Bienestar de la Familia case managers are county employees whose role includes coordinating care for people who need help safely quarantining or isolating. Bienestar de la Familia has a strong rapport with the Latinx and Spanish-speaking community as well as other communities of color, and provides isolation and quarantine assistance to people disproportionately impacted by the pandemic. Case managers work with clients to determine what services they need, and collaborate with other Bienestar staff who work on coordinating payments and service delivery for grocery, utility, and rent/mortgage assistance. Case managers also provide emotional support and help clients navigate other and longer-term social supports.
The system is complicated
The current wraparound service system to support isolation and quarantine goes through many county divisions and involves various external partnerships. The figure below illustrates how a person who received a positive lab test for COVID-19 might move through the wraparound service system.
The current wraparound service system is complex
An individual needing isolation or quarantine assistance needs to communicate with various county divisions and external partners before receiving services.
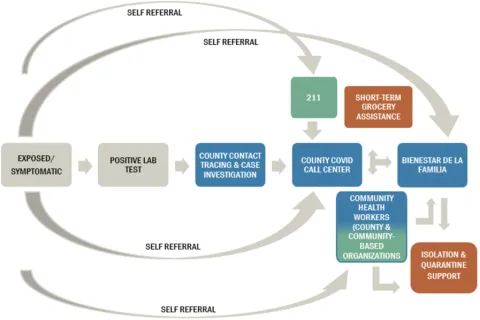
Source: Auditor's Office analysis of data, process charts, organizational charts, and interviews provided by Public Health and the Department of County Human Services.
A person may interact with Public Health, various programs within the Department of County Human Services such as the COVID Call Center and Bienestar, and with county partners such as community-based organizations. In theory, Public Health would contact a person who tests positive for COVID-19 a few days after testing positive. If the person indicated that they need assistance with isolating or quarantining, Public Health would then forward them to the COVID Call Center, where county staff would learn more about their specific needs and route them to either Bienestar de la Familia or a community health worker. If a caller needed immediate food assistance, staff at the COVID Call Center would also order groceries for same or next-day delivery so that households have food while they wait for additional services. Both Bienestar de la Familia and community-based organizations provided up to one month of grocery, utility, and rent/mortgage assistance. In some cases, community-based organizations referred clients back to Bienestar due to resource constraints.
County and partners delivered essential services, with more collaboration than in the past
The county and its partners supported thousands of people during the pandemic. Between June 01, 2020 and January 31, 2022, the county placed approximately 7,500 referrals to community health workers working with culturally and linguistically specific communities. Bienestar de la Familia responded to approximately 7,100 referrals as well. The COVID-19 Call Center also coordinated approximately 2,500 orders for urgent grocery assistance, which is defined as a household needing food within the next five days. While the COVID Call Center attempts to track self-referrals to community-based organizations, information received about self-referrals is at times limited because some organizations do not report self-referrals to the county. Based on reports from community-based organizations as well as missing information, the number of self-referrals that community-based organizations assisted may be higher than reported to the COVID Call Center. Requests for assistance of all types appeared to increase during surges, particularly during the Delta and Omicron surges.
The County and partners responded to thousands of referrals
Approximate number of referrals placed between June 01, 2020 and January 31, 2022.
Self-referrals placed to community-based organizations may be higher than reported.
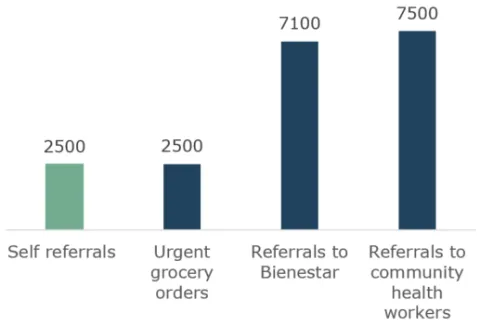
Source: Wraparound data from the COVID Call Center.
County staff and partners working directly with people reported that wraparound services have been successful in assisting people to isolate or quarantine. We also heard that communities have benefitted from working with case managers and community health workers who have been able to provide culturally-specific services. For example, Bienestar de la Familia conducted a survey with service recipients. According to their survey, 97% of survey respondents expressed satisfaction, and reported that the services they received improved their situation.
- “I appreciated how the people I worked with treated me with dignity and understanding. The program really helped me in my time of need. I am truly grateful.”
- “This is a true blessing during such a difficult time. I appreciate everyone's that helped me so much. I was worried about how we were gonna keep up with rent and bills and not to mention food. Words cannot explain how thankful I am for you guys.”
- “They were able to help me when I most needed. The food delivery was a life saver.”\
About 3% of respondents indicated that Bienestar services did not help or they were unsure if they helped. They cited needing longer term or additional services, as well as delays in service delivery.
- “One month's rent assistance is not enough. Assistance takes forever to help people cover their needs.”
Overall, during interviews we heard positive feedback and stories from various communities, community partners, and county staff alike.
- County staff praised the interdepartmental collaboration between Health and the Department of County Human Services. Staff remarked that they had not seen such a high level of coordination between departments in the 10+ years they have worked at the county.
- The county's relationships with community-based organizations were strengthened throughout the course of the pandemic. Public Health went from having partnerships with 17 community-based organizations to working with over 50. Many smaller community-based organizations now collaborate with the county on culturally-specific work.
- Community-based organizations and community leaders also strengthened relationships amongst themselves. Culturally-specific community-based organizations connected with one another and formed partnerships to share information, experiences, and troubleshoot. Community health workers from various organizations were able to connect with one another for support and training. Community leaders also formed and strengthened groups that do community advocacy and engagement work, like the Future Generations Collaborative and Lideres Naturales.
Dependence on phone calls and lack of advertising may have created access issues
The wraparound service system is highly dependent on phone calls. County staff and partners' primary form of contact with people is through phone calls, text messages, and voicemails. Likewise, people who have tested positive for COVID-19, have COVID-19 symptoms, or are close contacts of people who have COVID-19 must make and answer many phone calls in order to receive support services for quarantine or isolation. The service system places the onus on sick people to make and answer various phone calls. We heard that multiple phone calls led to caller fatigue, and for some people the process was confusing and overwhelming because they were talking to so many different people.
Sick or symptomatic people who were not contacted by the county may have also struggled to receive support services. People can also contact the county and partners directly as self-referrals. However, the county and partners did not publicize many avenues for self-referrals. A person in need of assistance might contact a community health worker or case manager directly by getting their phone number from a family member or friend.
Throughout much of the pandemic, the county instructed people who were interested in receiving wraparound services to contact 211. People who called 211 were given the number to the COVID Call Center. To date, there are still county communications instructing people to call 211 for assistance with isolation and quarantine. Calling 211 appeared to be an unnecessary step. This extra step may have contributed to caller fatigue and unnecessary complexity during a time-sensitive and stressful period. The COVID Call Center's number has been more widely advertised across county communications since January 2022.
People who need language translation services likely have additional difficulties connecting with service providers. County staff and partners frequently use third-party translation services. Support service coordinators may have to place several calls to successfully get translators and clients on the same phone call, which may further delay service delivery.
Data issues create challenges with service tracking and delivery
The wraparound service program's data systems have created challenges and risks. The systems were set up to be used on a temporary basis. There is limited data sharing and tracking that affects internal coordination as well as service delivery.
Community-based organizations have faced significant capacity constraints throughout the pandemic, and the current model for tracking their capacity may place unneeded strain on these organizations. Currently, community-based organizations submit capacity updates to the COVID Call Center and Public Health via various Google Forms, which includes an estimate of the number of county referrals they can accept at any given time. When the COVID Call Center makes a referral to a community-based organization, they must confirm their acceptance via individual e-mails. The current referral and capacity tracking system was set up during an emergency. At the same time, it is not the most efficient way to communicate with staff at community-based organizations that have been reporting capacity and resource challenges throughout the pandemic.
In addition, the county collects limited metrics from community-based organizations. Originally, the county made contracts with community-based organizations flexible so that they could pivot throughout the pandemic response. While this approach may have been beneficial, it also comes with various trade-offs related to measuring the efficiency and effectiveness of service delivery. Staff from some community-based organizations told us that the county never told them what data to collect, and many set up their own systems for tracking service delivery and communications. This means that the data may be difficult to aggregate in the future, or it may have reliability issues. Similar to contact tracing and outbreak investigation, we could not get sufficient data to assess wraparound services taking place at community-based organizations.
There are also various limitations with the county's approach to monitoring and coordinating services. Most notably, there is no form of data tracking and sharing that the county and partners can simultaneously access. This had led to:
- No monitoring of duplication of services - people may place requests for services at multiple organizations for the same time period, which limits resources and capacity to serve a greater number of people or provide more appropriate long-term assistance to the caller.
- Limited tracking of receipt of services - the county and partners make payments for grocery, utility, and rent assistance, but do not consistently confirm when landlords receive payments or when grocery deliveries are made. At times, this had led to clients following up with the county and partners to inform them that they have not received a particular service.
- No tracking of the timeliness of services - the county and partners do not have a way of looking up the average time of service delivery. While delivery of grocery and utility assistance appears to happen quickly, delivery of rent and mortgage assistance has been slow, particularly during high times of need like surges.
County's experience with contact tracing can provide lessons for future emergencies
Multnomah County's pandemic response happened quickly and during a moving crisis. This section draws on lessons learned to inform current and future county operations. While the next crisis may not look the same, past experiences can still be instructive. Most notably, the COVID-19 pandemic affects the whole county, not just one department. To better prepare for future emergencies, the county could prepare to stand up new programs quickly and continue to build capacity for community partnerships.
County can be better prepared to stand up new programs quickly
The county faced challenges with standing up and supporting the pandemic response programs involved in this audit. In the future, county leadership can better support new and expanded programs by utilizing the technical support and expertise that already exist at the county. Throughout this audit, we heard about two key areas in which programs could have benefitted from existing county resources: Human Resources and program set up.
Better onboarding and additional support could have helped
New and expanded programs struggled with staffing up quickly. We heard in interviews that new hires received technical training, but were not adequately trained on county culture, expectations, and processes. In addition, new supervisors and managers did not have sufficient training on the stipulations of union contracts, which may have contributed to union grievances and protected class complaints.
The county offers a welcome training for new staff and an orientation for new managers. Some departments also offer department-specific orientations. However, these trainings are not always available on demand and are not tailored to an emergency environment. We heard that having ready-made training materials for new workers and managers in an emergency could be especially helpful.
Additionally, Health Department human resources staff were overworked during the pandemic. The county lacks processes to redeploy county experts across departments to programs in need of support. We heard that people did not know who to ask for help. Even getting support with small things like data entry could have been beneficial. Some county staff were working long hours while staff in other departments were not asked to help.
Data and oversight systems could have been setup more effectively
COVID-19 response programs were set up quickly during a crisis. Possibly due to the crisis and quick timing, data systems were not set up to efficiently collect and store data that could facilitate oversight and evaluation.
The county does not have reliable, quantitative data about wraparound services, contact tracing, or outbreak investigation that spans the whole pandemic. We heard that the county considered purchasing a data system for wraparound services. Management decided not to obtain a new system because of the time it would take to set up. The program set up various temporary systems instead. However, the lack of an efficient system has created more work for county staff and staff at community-based organizations, as well as disorganized data.
Moving forward, the county should prioritize setting up effective data systems, with the consideration of being able to evaluate programs in the future. New systems do not have to be complex or collect a burdensome amount of data. Setting up data systems should focus on reducing staff burdens and collecting enough data in an organized way to facilitate evaluation.
County can build on experiences with community and cross-departmental partnerships
Public Health greatly expanded partnerships with community-based organizations as part of the pandemic response. The coordination and partnership work fell primarily to a small team in the Health Department called Community Partnerships and Capacity Building. The Racial and Ethnic Approaches to Community Health (REACH) program was also involved in community partnerships and outreach. The Emergency Operations Center also set up a network of liaisons to reach different communities and sectors. The county could expand capacity for this type of work more broadly and allow for greater cross-departmental collaboration, especially in times not in an emergency.
We heard that the partner organizations really appreciated the collaboration and the relationships with the Community Partnerships and Capacity Building team. However, we also heard that some organizations, particularly small ones that had not done direct service before, could have benefited from more technical assistance and guidance.
The county has an opportunity to continue to maintain relationships and support community-based organizations, even outside of the pandemic. Continued relationship building and adequate support will be important.
Many departments in the county contract with and work with community-based organizations. Having an internal network in place of people who do community partnership work will put the county in a better position to work with a broad array of community organizations in future emergencies. One possibility is a community of practice, or something similar, that would allow county employees to network and share expertise.
During the pandemic, the county translated materials into the five most commonly spoken languages throughout the county, though other materials were translated into up to 22 languages. Language translation can facilitate outreach and provide essential information to communities. However, language translation was not always done consistently and was driven by request. Other jurisdictions, such as the City of Seattle, have set translation standards for different circumstances. Setting standards could relieve communities from having to request language translation on a case-by-case basis and increase consistency.
County can involve stakeholders sooner and provide better guidance
Throughout interviews in this audit, we heard from some stakeholders and partners that they would have liked to be involved in meetings and decisions sooner in the pandemic response. It can be very challenging to involve everyone during a crisis. However, getting input from county experts in county functions sooner could have improved processes and avoided confusion. Getting input from county staff and partners with experience and understanding of the needs of different populations could have helped with service design. Involving stakeholders and partners also helps with buy-in.
Public Health could have also provided additional guidance and support with purchasing. Public Health created a list for providers on what expenses were allowable. However, we heard from both county staff and partners that they had been unclear on what items could and could not be purchased for wraparound support services, like grocery assistance. This led to confusion and additional time taken to clarify allowable expenses, which may have impacted efficiency and service delivery. Getting questions clarified at the county could also be cumbersome, because multiple people are involved with the determination process.
County should incorporate lessons learned for the future
The Health Department and county as a whole should look for opportunities to incorporate these lessons learned in the future. Implementing some activities, like developing onboarding materials, is straightforward. Other changes, like drawing on experts from other departments, are less straightforward to implement. Changes in county culture that bridge silos between departments and reinforce a culture of public service could help. However, a culture of public service alone is not sufficient. If people see that those working in the emergency response are working long hours or have other hardships, they may reasonably be reluctant to volunteer to participate. Union agreements also complicate reassigning staff that are represented by a union. In California, there is a law that designates all government employees as disaster service workers who can be reassigned during an emergency.
There may be opportunities to incorporate lessons learned into planning documents as well. Management reported that the county takes an "all-hazards" approach to emergencies and does not have a pandemic-specific response plan. The county does have an all-hazards emergency response plan. However, the public health portion of that all-hazards plan is out of date and not publicly available. This plan or another planning document may provide another place to document lessons learned.
Recommendations
Recommendations for the Health Department:
To provide better oversight and support to community-based organizations contracted to provide wraparound services, we recommend that the Health Department work with the Department of County Human Services, no later than October 1, 2022, to:
- Provide education and technical support to partner organizations around county contracts, reporting requirements, and county expectations around data collection, monitoring, and service provision.
- Monitor whether contracted partners adhere to monthly reporting requirements and create a plan of action for when they do not.
And no later than January 1, 2023, to:
- Develop a plan to evaluate the efficacy and timeliness of wraparound services and assess the current data collection and information sharing system under that lens.
- Document lessons-learned and incorporate into planning documents, including lessons-learned identified in this report.
There is an opportunity to continue building county coordination with community partners, community-based organizations, and cross-departmental partners. We recommend that the Health Department, including Community Partnerships and Capacity Building in Public Health, work with county Organization Learning, no later than July 1, 2023, to:
- Create a mechanism, such as a community of practice, for staff across the county who work with community partners and community-based organizations to network, collaborate, and develop professionally.
Recommendations for the Chief Operating Officer:
To address challenges with rapidly staffing programs and scaling up during an emergency, we recommend that the Chief Operating Officer work with department leadership, including the Health Department Director, Human Resources, Risk Management, and Emergency Management, no later than July 1, 2023, to:
- Identify barriers and establish processes for redeploying county experts to programs in need during emergencies. This could include exploring changes to labor contract language or a county policy for all employees to be disaster workers, and identifying a strategic range of cross-county participants, like Health and HR, to include in emergency preparedness activities.
- Evaluate and revise or add to general county trainings to ensure they set expectations for working during emergencies and can be available on demand.
Objectives, Scope, & Methodology
The objectives of this audit were to:
- Describe how widespread disease transmission (surges) affects the county's case investigation, outbreak investigation, contact tracing, and wraparound services and determine how those programs responded.
- Determine how county leadership and management supported new or expanded programs for case investigation, outbreak investigation, contact tracing, and wraparound service provision.
To accomplish these objectives we:
- Conducted over 70 interviews, including interviews with community-based organizations, the Oregon Health Authority, the Multnomah Education Service District, and county staff and management from the Health Department, the Department of County Human Services, Emergency Management, the Joint Office of Homelessness Services, and Central Human Resources.
- Studied applicable laws, policies, intergovernmental agreements, interdepartmental agreements, and national, state, and local public health guidance.
- Researched best practices, relevant literature, public health dashboards, frameworks, and related audit reports.
- Reviewed contracts and MOUs with service providers.
- Reviewed program documentation.
- Reviewed the adopted budgets and financial data for FY2020 through FY2022, including the funding for specific programs under the Health Department and the Department of County Human Services.
- Took trainings on contact tracing, case investigation, and trauma-informed evaluation.
For this audit, we analyzed personnel data and used financial information for the time period of July 2020 through February 2022 from Workday, the County's enterprise resource planning system. We assessed the reliability of Workday's data by (1) comparing to other sources, (2) reviewing related documentation, including contractor audit reports, and (3) working with county officials to identify any data problems. We determined that the data were sufficiently reliable for the purposes of this report.
We also used information about wraparound service coordination and provision from the COVID Call Center for the time period of June 2020 through January 2022. Prior to January 2021, Public Health was responsible for collecting and monitoring wraparound data. We found that data from this time period is less reliable, as data entry was inconsistent. Staff at the COVID Call Center have worked to clean the data collected by Public Health to the extent possible. We found that the data was sufficiently reliable for approximations and the purposes of this report.
We used information on case investigation for the time period of February 2020 through January 2022 from Opera, the State of Oregon's case investigation database. Multnomah County Public Health receives case investigation from Opera through a shared data mart. We limited the scope of our use of this data to high-level summaries. Based on the assessment and processing of Opera data by the County's epidemiologists, our office has determined that the data were sufficiently reliable for the purposes of this report.
We were unable to obtain data from various sources that were central to our audit objectives. We were unable to obtain contact tracing data. The State of Oregon mandated Multnomah County to use the state databases Opera for case investigation and ARIAS for contact tracing. The State of Oregon does not share contact tracing data from ARIAS back with the county. In addition, we were unable to acquire sufficient data on outbreak investigation, which are logged in a subset of the state database Opera called DUDE. The State of Oregon does not share information in DUDE back with the county. We were also unable to acquire sufficient data from community-based organizations on the services they are contracted to provide. The county intentionally made contracts and reporting structures more lenient to provide flexibility during the pandemic response. Due to these limitations, we were unable to confidently and quantitatively assess the impacts of surges on contact tracing, outbreak investigation, and contracted wraparound services.
We conducted this performance audit in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings, and conclusions based on our audit objective. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Audit Staff
Caroline Zavitkovski, CIA, Principal Management Auditor
Dorian Pacheco, Management Auditor
